the autolytic debridement of venous leg ulcers - Wounds International
the autolytic debridement of venous leg ulcers - Wounds International
the autolytic debridement of venous leg ulcers - Wounds International
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Technical Guide<br />
THE AUTOLYTIC DEBRIDEMENT<br />
OF VENOUS LEG ULCERS<br />
Deborah H<strong>of</strong>man is Clinical Nurse Specialist in Wound Healing, Department <strong>of</strong> Dermatology, Churchill Hospital, Oxford<br />
Wound <strong>debridement</strong> is part <strong>of</strong> <strong>the</strong> wound healing process which may occur without intervention but,<br />
more <strong>of</strong>ten, assistance is needed. It is important to recognise <strong>the</strong> situations when <strong>debridement</strong> is not<br />
appropriate. This article will describe how to recognise dead tissue that should be removed from <strong>the</strong><br />
wound, when <strong>debridement</strong> should not be attempted and <strong>the</strong> various methods that can be used.<br />
Debridement describes any<br />
method that facilitates <strong>the</strong><br />
removal <strong>of</strong> dead (necrotic) tissue,<br />
cell debris or foreign bodies from<br />
a wound (O’Brien, 2003). It is<br />
regarded as an essential part<br />
<strong>of</strong> wound bed preparation, as<br />
it enhances <strong>the</strong> potential for a<br />
wound to heal. Dead tissue in<br />
<strong>the</strong> wound not only physically<br />
prevents <strong>the</strong> wound from<br />
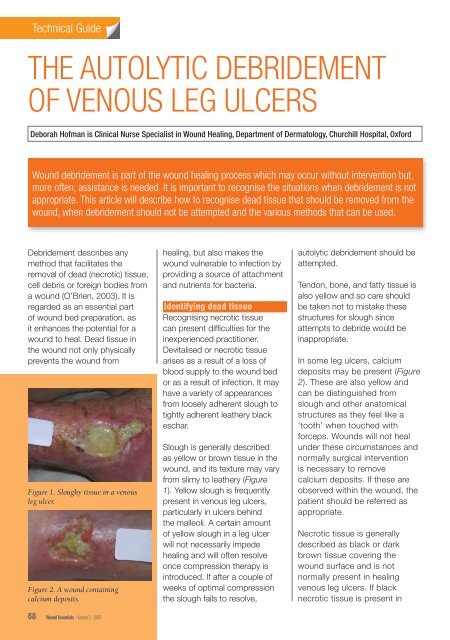
Figure 1. Sloughy tissue in a <strong>venous</strong><br />
<strong>leg</strong> ulcer.<br />
Figure 2. A wound containing<br />
calcium deposits.<br />
68 Wound Essentials • Volume 2 • 2007<br />
healing, but also makes <strong>the</strong><br />
wound vulnerable to infection by<br />
providing a source <strong>of</strong> attachment<br />
and nutrients for bacteria.<br />
Identifying dead tissue<br />
Recognising necrotic tissue<br />
can present diffi culties for <strong>the</strong><br />
inexperienced practitioner.<br />
Devitalised or necrotic tissue<br />
arises as a result <strong>of</strong> a loss <strong>of</strong><br />
blood supply to <strong>the</strong> wound bed<br />
or as a result <strong>of</strong> infection. It may<br />
have a variety <strong>of</strong> appearances<br />
from loosely adherent slough to<br />
tightly adherent lea<strong>the</strong>ry black<br />
eschar.<br />
Slough is generally described<br />
as yellow or brown tissue in <strong>the</strong><br />
wound, and its texture may vary<br />
from slimy to lea<strong>the</strong>ry (Figure<br />
1). Yellow slough is frequently<br />
present in <strong>venous</strong> <strong>leg</strong> <strong>ulcers</strong>,<br />
particularly in <strong>ulcers</strong> behind<br />
<strong>the</strong> malleoli. A certain amount<br />
<strong>of</strong> yellow slough in a <strong>leg</strong> ulcer<br />
will not necessarily impede<br />
healing and will <strong>of</strong>ten resolve<br />
once compression <strong>the</strong>rapy is<br />
introduced. If after a couple <strong>of</strong><br />
weeks <strong>of</strong> optimal compression<br />
<strong>the</strong> slough fails to resolve,<br />
<strong>autolytic</strong> <strong>debridement</strong> should be<br />
attempted.<br />
Tendon, bone, and fatty tissue is<br />
also yellow and so care should<br />
be taken not to mistake <strong>the</strong>se<br />
structures for slough since<br />
attempts to debride would be<br />
inappropriate.<br />
In some <strong>leg</strong> <strong>ulcers</strong>, calcium<br />
deposits may be present (Figure<br />
2). These are also yellow and<br />
can be distinguished from<br />
slough and o<strong>the</strong>r anatomical<br />
structures as <strong>the</strong>y feel like a<br />
‘tooth’ when touched with<br />
forceps. <strong>Wounds</strong> will not heal<br />
under <strong>the</strong>se circumstances and<br />
normally surgical intervention<br />
is necessary to remove<br />
calcium deposits. If <strong>the</strong>se are<br />
observed within <strong>the</strong> wound, <strong>the</strong><br />
patient should be referred as<br />
appropriate.<br />
Necrotic tissue is generally<br />
described as black or dark<br />
brown tissue covering <strong>the</strong><br />
wound surface and is not<br />
normally present in healing<br />
<strong>venous</strong> <strong>leg</strong> <strong>ulcers</strong>. If black<br />
necrotic tissue is present in
Technical Guide<br />
a <strong>leg</strong> ulcer, o<strong>the</strong>r causes <strong>of</strong><br />
ulceration should be looked<br />
for, e.g. ischaemia (Figure 3),<br />
in which case urgent referral<br />
to a vascular unit should<br />
be instigated. Pyoderma<br />
gangrenosum and vasculitis are<br />
relatively rare conditions which<br />
cause <strong>leg</strong> ulceration and <strong>of</strong>ten<br />
cause necrosis. In patients<br />
with vasculitis, <strong>the</strong>re are usually<br />
mulitple lesions present (Figure<br />
4). Pyoderma gangrenosum<br />
usually presents as a rapidly<br />
enlarging, very painful lesion<br />
with necrosis and typically <strong>the</strong>re<br />
is undermining at <strong>the</strong> wound<br />
edges (Figure 5). Patients where<br />
<strong>the</strong>se conditions are suspected<br />
should undergo urgent referral<br />
to a dermatologist.<br />
Slough which is heavily<br />
colonised with anaerobic<br />
bacteria is also <strong>of</strong>ten black.<br />
However, this is usually slimy,<br />
as opposed to <strong>the</strong> dry lea<strong>the</strong>ry<br />
texture <strong>of</strong> necrotic tissue, and<br />
can be effectively managed<br />
with topical metronidazole.<br />
Topical metronidazole can be<br />
used safely on wounds for<br />
up to six weeks. There is no<br />
known risk <strong>of</strong> resistance or<br />
contact sensitivity. However, in<br />
patients who are taking warfarin,<br />
it should be used with care<br />
as it affects <strong>the</strong> international<br />
normalised ratio (INR).<br />
Dried blood on <strong>the</strong> wound<br />
surface is also black and may<br />
be difficult to distinguish from<br />
necrotic tissue.<br />
It is important to be able to<br />
recognise and describe different<br />
types <strong>of</strong> tissue and to know<br />
when to leave well alone. If in<br />
doubt specialist help should<br />
always be sought.<br />
70 Wound Essentials • Volume 2 • 2007<br />
Figure 3. Necrotic tissue in ulcer with significant arterial insufficiency.<br />
Figure 4. Vasculitis.<br />
Figure 5. Pyoderma gangrenosum.<br />
Selecting a method<br />
<strong>of</strong> <strong>debridement</strong><br />
The selection <strong>of</strong> a method<br />
<strong>of</strong> <strong>debridement</strong> depends on<br />
<strong>the</strong> availability <strong>of</strong> product,<br />
local expertise and patient<br />
preference.<br />
There are a number <strong>of</strong><br />
<strong>debridement</strong> techniques used by
healthcare pr<strong>of</strong>essionals, and<br />
<strong>the</strong>y can be categorised into:<br />
8Active <strong>debridement</strong><br />
8Autolytic <strong>debridement</strong> (ei<strong>the</strong>r<br />
moisture donating or moisture<br />
absorbing).<br />
Active <strong>debridement</strong><br />
Surgical <strong>debridement</strong><br />
Surgical <strong>debridement</strong> involves<br />
<strong>the</strong> removal <strong>of</strong> dead tissue from<br />
<strong>the</strong> wound bed. It is carried out<br />
under surgical conditions and<br />
results in a bleeding wound bed<br />
as a result <strong>of</strong> complete removal <strong>of</strong><br />
necrotic material. This is carried<br />
out by surgeons, podiatrists and<br />
specialist nurses who have been<br />
trained in <strong>the</strong> procedure, using<br />
scalpel and forceps.<br />
Sharp <strong>debridement</strong><br />
Sharp <strong>debridement</strong> is <strong>the</strong> removal<br />
<strong>of</strong> dead tissue with scissors<br />
or scalpel. This should only<br />
be carried out by a healthcare<br />
pr<strong>of</strong>essional who has been<br />
trained in <strong>the</strong> procedure.<br />
Larval <strong>the</strong>rapy<br />
Larvae or maggots have been<br />
used in <strong>the</strong> UK to debride<br />
wounds for at least 10 years<br />
and are a fast, effective and<br />
safe method <strong>of</strong> <strong>debridement</strong><br />
(Thomas, 1998). Maggots are<br />
now available ei<strong>the</strong>r as ‘freerange’<br />
(and placed directly into<br />
<strong>the</strong> wound) or contained in<br />
bags. The powerful enzymes<br />
in <strong>the</strong>ir saliva dissolve necrotic<br />
tissue, which <strong>the</strong> maggots <strong>the</strong>n<br />
ingest. They do not have to be<br />
in direct contact with <strong>the</strong> wound<br />
bed. However, free-range<br />
maggots have <strong>the</strong> advantage<br />
<strong>of</strong> being able to penetrate<br />
crevices and sinuses more<br />
effectively. The disadvantage is<br />
that <strong>the</strong>y can escape and cause<br />
distress to both patient and<br />
practitioner. A detailed guide to<br />
larval <strong>the</strong>rapy can be found on<br />
p.156–9.<br />
Enzymatic<br />
There are various enzyme<br />
preparations which are effective<br />
at digesting dead tissue, e.g.<br />
collagenase and papaina, but<br />
<strong>the</strong>se are not currently available<br />
in <strong>the</strong> UK (Bellingeri and H<strong>of</strong>man,<br />
2006).<br />
Autolytic <strong>debridement</strong><br />
Autolytic <strong>debridement</strong> is <strong>the</strong><br />
process by which <strong>the</strong> body<br />
attempts to shed devitalised<br />
tissue by <strong>the</strong> use <strong>of</strong> moisture.<br />
Where tissue can be kept moist,<br />
it will naturally degrade and<br />
deslough from <strong>the</strong> underlying<br />
healthy structures. This process<br />
is helped by <strong>the</strong> presence<br />
<strong>of</strong> enzymes called matrix<br />
metalloproteinases (MMPs),<br />
which are produced by damaged<br />
tissue and which disrupt <strong>the</strong><br />
proteins that bind <strong>the</strong> dead tissue<br />
to <strong>the</strong> body. This process can<br />
be enhanced by <strong>the</strong> application<br />
<strong>of</strong> wound management<br />
products which promote a moist<br />
environment. These products can<br />
be divided into two categories:<br />
those that donate moisture<br />
to <strong>the</strong> dead tissue and those<br />
that absorb excess moisture<br />
produced by <strong>the</strong> body. Both are<br />
designed to facilitate <strong>the</strong> <strong>autolytic</strong><br />
<strong>debridement</strong> process (Gray et al,<br />
2005).<br />
Moisture donation<br />
Hydrocolloids and hydrogels<br />
(amorphous gel in a tube or<br />
hydrogel sheets), donate moisture<br />
to <strong>the</strong> dead tissue to facilitate<br />
<strong>autolytic</strong> <strong>debridement</strong>.These<br />
dressings are particularly useful<br />
in wounds that are not heavily<br />
exuding (Tip 1).<br />
Technical Guide<br />
The use <strong>of</strong> a second generation<br />
hydrogel sheet, e.g. Actiform<br />
Cool ® , will absorb a certain<br />
amount <strong>of</strong> moisture while<br />
donating it so, in many cases,<br />
will provide a good moisture<br />
balance at <strong>the</strong> wound surface.<br />
If desired <strong>the</strong> dressing can be<br />
cut to fit <strong>the</strong> wound (Tip 2). The<br />
white backing should be peeled<br />
<strong>of</strong>f and <strong>the</strong> dressing laid gel side<br />
down on to <strong>the</strong> wound surface.<br />
Dressings should be changed<br />
when <strong>the</strong>re is strikethrough, but<br />
may be left on for up to seven<br />
days if <strong>the</strong>re is no leakage. A<br />
second generation hydrogel sheet<br />
dressing may continue to be used<br />
after <strong>debridement</strong> has occurred<br />
through to healing as it promotes<br />
granulation tissue and maintains a<br />
clean wound bed (Figures 6,7,8,9).<br />
Moisture absorption<br />
Alginates, cellulose dressings and<br />
foams are designed to absorb<br />
exudate. By absorbing excess<br />
wound fluid, <strong>the</strong>se products<br />
avoid damage to <strong>the</strong> surrounding<br />
skin from maceration (Tip 3).The<br />
structure <strong>of</strong> some foam dressings<br />
alters under compression so that<br />
<strong>the</strong> moisture remains in contact<br />
with <strong>the</strong> skin. Care should be<br />
taken <strong>the</strong>refore to select an<br />
appropriate foam. These dressings<br />
Tip 1<br />
8A common error is to apply<br />
a hydrogel to a wet wound<br />
that contains some slough<br />
in an attempt to debride <strong>the</strong><br />
wound. It is more important<br />
to get <strong>the</strong> moisture balance<br />
right than to remove <strong>the</strong><br />
sloughy tissue which will<br />
resolve itself in <strong>the</strong> right<br />
environment.<br />
Wound Essentials • Volume 2 • 2007 71
Technical Guide<br />
Figure 6. Slough is present on <strong>the</strong> wound<br />
bed before application <strong>of</strong> dressing.<br />
Figure 7. Remove <strong>the</strong> backing from <strong>the</strong><br />
hydrogel sheet and place gel side down<br />
on <strong>the</strong> wound.<br />
Figure 8. A clean wound bed on removal<br />
<strong>of</strong> <strong>the</strong> dressing.<br />
Figure 9. Once <strong>debridement</strong> has<br />
occurred, <strong>the</strong> dressing can be continued<br />
to promote granulation.<br />
should not be used on a dry<br />
sloughy wound as <strong>the</strong>y will fur<strong>the</strong>r<br />
dry out <strong>the</strong> tissue, making it more<br />
adherent and painful.<br />
Dressings which reduce <strong>the</strong><br />
bacterial burden <strong>of</strong> <strong>the</strong> wound<br />
A heavy bacterial burden in<br />
a wound will encourage tissue<br />
72 Wound Essentials • Volume 2 • 2007<br />
degradation and slough formation.<br />
Dressings which reduce bacteria in<br />
a wound such as honey, silver, or<br />
cleansing fluid such as Prontosan ®<br />
(Horrocks, 2006), may help to<br />
reduce slough and promote healthy<br />
granulation.<br />
The process <strong>of</strong> <strong>debridement</strong><br />
will increase exudate and this in<br />
turn may damage surrounding<br />
skin. The frequency <strong>of</strong> dressing<br />
change may have to be<br />
increased and surrounding<br />
skin protected with a suitable<br />
barrier such as Cavilon cream/<br />
ointment (3M Health Care) or<br />
zinc paste. Dressings which<br />
donate moisture (such as<br />
hydrogels) should not be used<br />
on a wet wound as <strong>the</strong> increase<br />
in moisture will macerate <strong>the</strong><br />
skin. Honey dressings, although<br />
increasing exudate in <strong>the</strong> initial<br />
phase, will, by reducing bacterial<br />
load, also eventually reduce<br />
exudate.<br />
The choice <strong>of</strong> method <strong>of</strong><br />
<strong>debridement</strong> depends on wound<br />
severity and patient preference.<br />
Many patients like <strong>the</strong> idea <strong>of</strong> a<br />
natural product such as honey. The<br />
only reason to avoid this dressing<br />
would be pain as patients <strong>of</strong>ten find<br />
<strong>the</strong> drawing sensation intolerable.<br />
Maggot treatment is more rapid<br />
than <strong>autolytic</strong> <strong>debridement</strong> and if<br />
<strong>the</strong> wound is very <strong>of</strong>fensive and<br />
<strong>the</strong>re is a lot <strong>of</strong> sloughy/necrotic<br />
tissue <strong>the</strong> larval <strong>the</strong>rapy should<br />
be considered.<br />
If <strong>the</strong> wound is very painful it is<br />
unlikely that maggot treatment will<br />
be tolerated, and some patients<br />
are repelled by <strong>the</strong> idea <strong>of</strong> larval<br />
<strong>the</strong>rapy. In a painful wound,<br />
<strong>the</strong> use <strong>of</strong> a second generation<br />
hydrogel sheet should be<br />
considered.<br />
Common misconceptions<br />
8Practitioners are rightly<br />
taught that <strong>debridement</strong> is an<br />
essential part <strong>of</strong> wound healing.<br />
However, dressings which are<br />
marketed as having a debriding<br />
action, e.g. hydrogels, are <strong>of</strong>ten<br />
applied inappropriately without<br />
consideration <strong>of</strong> moisture<br />
balance. This can result in<br />
maceration.<br />
8In an attempt to debride<br />
wounds on wet <strong>leg</strong> <strong>ulcers</strong>,<br />
<strong>the</strong> healthcare pr<strong>of</strong>essional<br />
<strong>of</strong>ten uses a combination <strong>of</strong><br />
dressings which are <strong>the</strong>reby<br />
rendered ineffective, e.g.<br />
hydrogels (moisture donating)<br />
and alginates (moisture<br />
absorbing) or hydrogels and<br />
foams (moisture absorbing). A<br />
combination <strong>of</strong> <strong>the</strong>se dressings<br />
results in a ‘sludge’ which has<br />
no debriding effect.<br />
Where <strong>the</strong> wound is very<br />
wet <strong>the</strong> practitioner should<br />
attempt to identify <strong>the</strong><br />
Tip 2<br />
8Patients should be warned<br />
that <strong>the</strong> constituency <strong>of</strong><br />
<strong>the</strong> second generation<br />
hydrogel sheet dressing will<br />
change and <strong>the</strong>re may be<br />
an unpleasant odour. This<br />
is also true <strong>of</strong> hydrocolloid<br />
dressings.<br />
Tip 3<br />
8Capillary action dressings or<br />
those with a super absorbent<br />
capability may be useful in<br />
<strong>the</strong> management <strong>of</strong> very wet<br />
sloughy wounds.
cause and address moisture<br />
balance before considering<br />
<strong>debridement</strong>. Possible causes<br />
<strong>of</strong> wetness include:<br />
1. Heavy bacterial burden: Does<br />
<strong>the</strong> patient need systemic<br />
antibiotics and/or topical<br />
antibacterial management (e.g.<br />
honey, silver, iodine)?<br />
2. Wet eczema: does <strong>the</strong> patient<br />
need referral to a specialist<br />
nurse or dermatologist?<br />
Topical steroid <strong>the</strong>rapy may be<br />
needed.<br />
2. Oedema: Is <strong>the</strong> patient<br />
receiving adequate<br />
compression? Are <strong>the</strong>y<br />
elevating <strong>the</strong>ir <strong>leg</strong>s sufficiently?<br />
Have <strong>the</strong>y been taught<br />
dorsiflexion exercises to reduce<br />
oedema?<br />
3. Is <strong>the</strong> dressing sufficiently<br />
absorbent? Dressings within<br />
<strong>the</strong> same category perform<br />
differently, e.g. foams. Some<br />
will remove <strong>the</strong> exudate<br />
from <strong>the</strong> wound, but o<strong>the</strong>rs<br />
keep <strong>the</strong> exudate next to<br />
<strong>the</strong> skin causing fur<strong>the</strong>r<br />
tissue damage. Many foams<br />
do not perform well under<br />
compression. Alginates and<br />
cellulose (Aquacel ®, ConvaTec)<br />
dressings can be beneficial. If<br />
<strong>the</strong>re is heavy pseudomonal<br />
exudate, which has a<br />
characteristic bright green<br />
colour, dressings containing<br />
silver may be helpful.<br />
When is debriding a <strong>venous</strong> <strong>leg</strong><br />
ulcer not appropriate?<br />
1. Arterial <strong>ulcers</strong> should not<br />
normally be debrided (Leaper,<br />
2002). If <strong>the</strong>re is a poor blood<br />
supply to <strong>the</strong> limb, it is best to<br />
keep a necrotic wound dry until<br />
seen by a vascular surgeon, as<br />
wet gangrene can occur.<br />
2. When diagnosis is in doubt.<br />
For example, pyoderma<br />
gangrenosum is characterised<br />
by rapid ulceration and<br />
necrosis. Debridement is<br />
contraindicated as it may<br />
cause extension <strong>of</strong> <strong>the</strong><br />
ulceration (Chakrabarty and<br />
Philips, 2002).<br />
3. The <strong>debridement</strong> <strong>of</strong> malignant<br />
wounds serves no useful<br />
purpose and may cause<br />
bleeding. If diagnosis is in<br />
doubt, specialist help should<br />
be sought.<br />
4. When <strong>the</strong> patient is<br />
systemically severely unwell,<br />
for example, in ITU or terminally<br />
ill. Local intervention is unlikely<br />
to help heal <strong>the</strong> wound and<br />
patient comfort ra<strong>the</strong>r than<br />
<strong>debridement</strong> should be<br />
a priority.<br />
Conclusions<br />
There are four questions that<br />
should be asked before making<br />
a decision on how to manage a<br />
sloughy/necrotic wound:<br />
1. Is <strong>the</strong> tissue in <strong>the</strong> wound<br />
definitely slough?<br />
2. Is <strong>debridement</strong> appropriate?<br />
3. What is causing <strong>the</strong> slough<br />
within <strong>the</strong> wound? Infection?<br />
Poor blood supply?<br />
4. Are <strong>the</strong> causes being<br />
addressed?<br />
5. In choosing dressings which<br />
promote <strong>debridement</strong>, has<br />
moisture balance and patient<br />
preference been considered?<br />
If in doubt specialist help must be<br />
sought. WE<br />
Bellingeri A, H<strong>of</strong>man D (2006)<br />
Debridement <strong>of</strong> pressure <strong>ulcers</strong>. In:<br />
Science and Practice <strong>of</strong> Pressure<br />
Ulcer Management. Springer–Verlag,<br />
London:129–39<br />
Chakrabarty A, Philips TJ (2002)<br />
Diagnostic Dilemmas:Pyoderma<br />
gangrenosum. <strong>Wounds</strong> 14(8): 302–5<br />
Glossary<br />
Technical Guide<br />
Autolysis: natural degradation <strong>of</strong> dead<br />
tissue in a wound.<br />
Calcification: calcium deposits which<br />
may occur in a <strong>leg</strong> ulcer.<br />
Debridement: removal <strong>of</strong> dead tissue<br />
from a wound.<br />
Necrotic tissue/necrosis: dead tissue<br />
which is desiccated usually dark<br />
brown or black.<br />
Slough: yellow or grey or brown<br />
in coulour, wet stringy tissue that<br />
adheres to <strong>the</strong> wound bed.<br />
Eschar: dry necrotic tissue.<br />
INR: <strong>the</strong> time taken for blood to clot<br />
compared to a control. Normal range<br />
is 0.9–1.2.<br />
Gray D, White R, Cooper P,<br />
Kingsley A (2005) Applied Wound<br />
Management. In: Wound Healing: A<br />
Systematic Approach to Advanced<br />
Wound Healing and Management.<br />
<strong>Wounds</strong> UK, Aberdeen: 59–96<br />
Horrocks A (2006) Prontosan wound<br />
irrigation and gel: management <strong>of</strong><br />
chronic wounds. Br J Nurs 15(22):<br />
1222–8<br />
Leaper D (2002) Sharp Techniques<br />
for Wound Debridement. World Wide<br />
<strong>Wounds</strong>, Dec 2002<br />
M<strong>of</strong>fatt C, Morison MJ, Pina E (2004)<br />
Wound bed preparation for <strong>venous</strong><br />
<strong>leg</strong> <strong>ulcers</strong>. In: European Wound<br />
Management Association (EWMA)<br />
Position Document: Wound Bed<br />
Preparation in Practice. MEP Ltd,<br />
London: 12–15<br />
Thomas S, Jones M, Andrews AM<br />
(1998) The use <strong>of</strong> larval <strong>the</strong>rapy in<br />
wound management. J Wound Care<br />
7(10): 521–4<br />
O’Brien M (2003) Exploring methods<br />
<strong>of</strong> wound <strong>debridement</strong>. In: White<br />
R, ed. Trends in Wound Care. Vol<br />
2. Quay books, MA Healthcare,<br />
London: 95–107<br />
Wound Essentials • Volume 2 • 2007 73