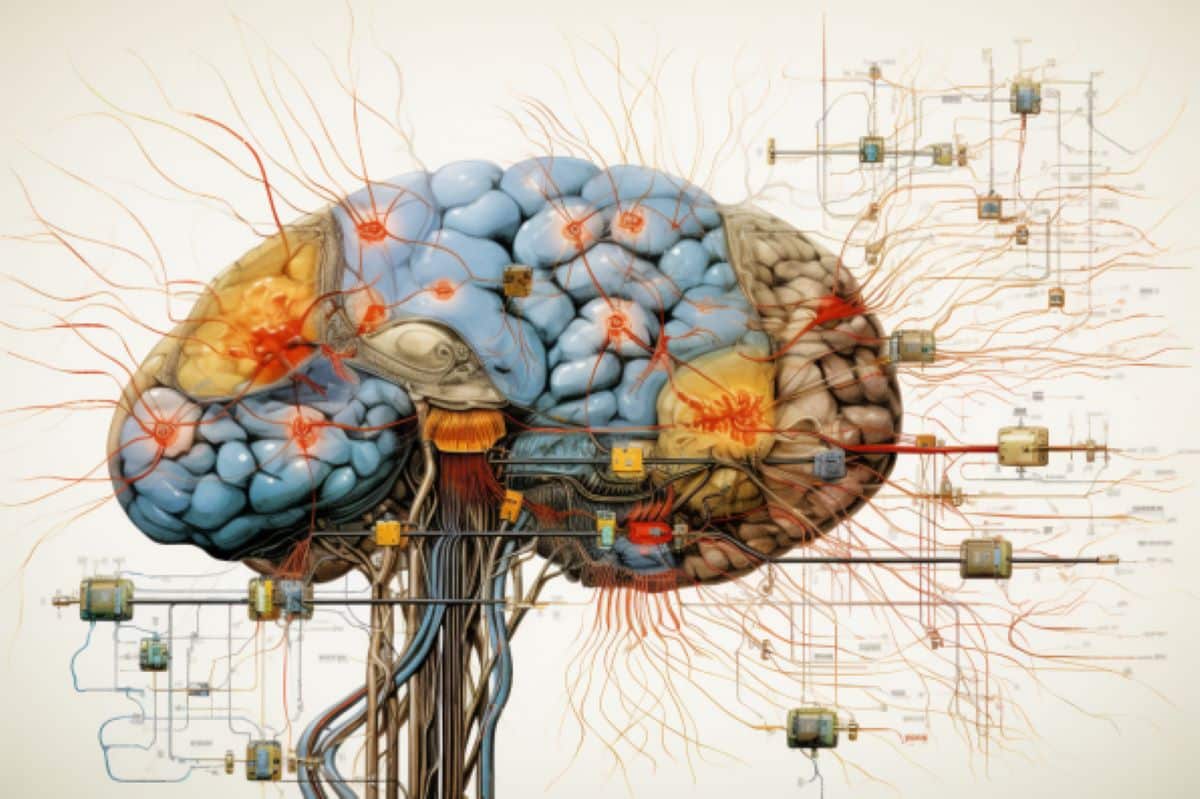
Summary: Researchers discovered a universal brain network present in people with substance use disorders. Analyzing data from over 144 studies involving 9,000+ participants, they found consistent abnormalities regardless of substance or lesion location. This commonality suggests a specific brain circuit that could be a therapeutic target for neurostimulation treatments.
Key Facts:
- The study evaluated data across 144 studies, revealing a consistent brain network abnormality in substance use disorders regardless of the type of substance or lesion.
- The research shows that regions previously thought to be individual targets for addiction treatments are part of a shared circuit.
- The findings support the idea of using targeted neurostimulation, like transcranial magnetic stimulation, to treat addiction.
Source: Brigham and Women’s Hospital
A new study by researchers at Brigham and Women’s Hospital, a founding member of the Mass General Brigham healthcare system, suggests a common brain network exists among people with substance use disorder.
By evaluating data from across more than 144 studies of addiction, the team found abnormalities across substance use disorders mapped to a common brain network across substances and lesion locations, suggesting a potential brain circuit to target with neurostimulation therapies.
The findings are published in Nature Mental Health.
“Our study found that different brain regions implicated in addiction are all a part of a common brain circuit,” said Michael Fox, MD, PhD, a corresponding author on the paper and founding director of the Center for Brain Circuit Therapeutics at Brigham and Women’s Hospital.
“Consistency across different papers means we now have a brain circuit to target addiction with treatments, rather than just a region.”
Fox collaborated with others in the Center for Brain Circuit Therapeutics as well as researchers from British Columbia, Boston Children’s Hospital, Wake Forest School of Medicine, and Philips Healthcare to complete the study.
The first author of the paper, Jacob Stubbs, PhD, is a medical student at the University of British Columbia. The study started when Stubbs was a visiting scholar at Brigham and Women’s Hospital under Fox.
The team looked at data from previous studies involving more than 9,000 participants. Within each of those studies, different brain regions were noted as a place to target to treat addiction.
“The best potential targets were unclear because of how many different abnormalities have been found across those previous studies,” Stubbs said.
Researchers used a network mapping approach with an average wiring diagram to find the link between the different types of brain imaging lesions that affect addiction. It also looked at different substances and found the network was common, whether someone was addicted to nicotine, alcohol, cocaine or heroin.
“What’s fascinating is that because there’s so much heterogeneity in the neuroimaging and substance use disorder literature, we thought it was unlikely that we’d find a common circuit. But after much work and collaboration, we found something,” Stubbs said. “It’s exciting science.”
One limitation to the study is because the data came from previous studies and the findings are correlative, the authors could not conclude causation. Stubbs also noted there are many ways to look at brain imaging, which makes looking at the data more complicated.
Fox said that despite the extensive data points, narrowing down a specific circuit fills in a gap from previous studies done in the Center for Brain Circuit Therapeutics, bringing targeted neurostimulation to treat addiction, like transcranial magnetic stimulation, closer to patients in a clinical setting.
“This study connects our previous work on lesions that stopped addiction to the last 50 years of research on neuroimaging abnormalities in patents with addiction,” Fox said.
Joseph Taylor, MD, PhD, a psychiatrist and clinical director of transcranial magnetic stimulation at the CBCT, and a co-author of the paper, said that unification is a huge step in the field of brain circuit therapeutics.
“This convergence boosts our confidence that we are starting to understand the circuitry of substance use disorders,” Taylor said.
Disclosures: CH is employed by BrainsWay and has financial interest in the company. SHS is a scientific consultant for Magnus Medical, and a clinical consultant for Acacia Mental Health, Kaizen Brain Center, and Boston Precision Neurotherapeutics. SHS has received investigator-initiated research funding from Neuronetics and BrainsWay.
SHS has served as a speaker for BrainsWay (branded) and PsychU.org (unbranded, sponsored by Otsuka). SHS owns stock in BrainsWay (publicly traded) and Magnus Medical (not publicly traded). SHS owns intellectual property involving the use of functional connectivity to target TMS.
MDF is a consultant for Magnus Medical, Solaris, and Boston Scientific and has intellectual property using connectivity imaging to guide brain stimulation. All other authors report no competing interests.
Funding: JLS was supported by a Canadian Institutes of Health Research Vanier Scholarship and a University of British Columbia Friedman Award for Scholars in Health. JJT was supported by the National Institute of Mental Health (K23MH129829), the Brain and Behavior Research Foundation, Sidney R. Baer Foundation, the Baszucki Brain Research Fund, and Harvard Medical School. FLWVJS was supported by the NIH (R01NS127892).
AC was supported by the NIH (K23MH120510), the Child Neurology Foundation, and the Simons Foundation. Data from the Rochester cohort was supported in part by the National Heart, Lung, and Blood Institute Preventive Cardiology Training Grant # T32 HL007937 and by the Clinical and Translational Science Institute Grant # UL1 RR024160 from the National Institutes of Health. WGH was supported by the Jack Bell Chair in Schizophrenia.
MDF was supported by grants from the NIH (R01MH113929, R21MH126271, R56AG069086, R21NS123813, R01NS127892), the Kaye Family Research Endowment, the Ellison / Baszucki Family Foundation, and the Manley Family.
About this addiction and neuroscience research news
Author: Cassandra Falone
Source: Brigham and Women’s Hospital
Contact: Cassandra Falone – Brigham and Women’s Hospital
Image: The image is credited to Neuroscience News
Original Research: Closed access.
“Heterogeneous neuroimaging findings across substance use disorders localize to a common brain network” by Michael Fox et al. Nature Mental Health
Abstract
Heterogeneous neuroimaging findings across substance use disorders localize to a common brain network
Substance use disorders are associated with neuroimaging abnormalities, but results are heterogeneous across studies and vary across substances, and the causal interpretation of these abnormalities is unknown.
We have used network mapping approaches and a functional connectome from a large cohort of healthy participants (n = 1,000) to test whether neuroimaging abnormalities across substance use disorders map to a common brain network.
Starting with coordinates of regional brain atrophy from 45 studies (3,791 participants), we found that 91% of the neuroimaging findings mapped to a common brain network. This network was specific to substance use disorder compared to atrophy associated with normal aging and neurodegenerative disease (PFWE < 0.05).
Coordinates of functional MRI abnormalities from 99 studies (5,256 participants) mapped to a similar brain network. We found no differences in networks across different substance use categories.
We combined all substance use disorder data (144 studies, 9,047 participants) to generate an overall coordinate-based network for substance use disorder, which included positive connectivity to the anterior cingulate, bilateral insulae, dorsolateral prefrontal cortices and thalamus, and negative connectivity to the medial prefrontal and occipital cortices.
Lesions resulting in remission from nicotine use disorder (n = 34) intersected this network significantly more than control lesions (n = 69; P < 0.0084).
We conclude that neuroimaging abnormalities across substance use disorders map to a common brain network that is similar across imaging modalities, substances and lesion locations that cause remission from substance use disorders.