Approach Considerations
The traditional basis of diagnosis is identifying Giardia intestinalis trophozoites or cysts in the stool of infected patients via a stool ova and parasite (O&P) examination. However, in relatively more recent years, the advent of more objective techniques (eg, immunoassays, nucleic acid amplification techniques [NAATs]) has led to an increase in their use, rather than those that rely on subjective microscopic examination of fecal specimens for Giardia cysts. [66]
Stool examination may be performed on fresh specimens or after preservation with polyvinyl alcohol or 10% formalin (with appropriate staining). Ideally, three specimens from different days should be examined because of potential variations in fecal excretion of cysts. G intestinalis is identified in 50-70% of patients after a single stool examination and in more than 90% after three stool examinations.
Stool O&P testing aids in the diagnosis of giardiasis in 80-85% of patients. It remains the diagnostic method with which other tests are compared. Aspiration of duodenal contents and demonstration of trophozoites has also been used for diagnosis, but this procedure is invasive and, in direct comparison studies to stool microscopy, may have a lower diagnostic yield.
Stool antigen enzyme-linked immunosorbent assays also are available. [67] These tests are similar to the stool O&P test in terms of cost and have a sensitivity of 88-98% and a specificity of 87-100%. These tests are best used as a screening test in high-incidence settings such as day-care centers or for identification of subjects during an epidemic, but they should not take the place of stool microscopy.
If the results from three O&P tests are negative and giardiasis is still suspected, stool antigen enzyme-linked immunosorbent assay (ELISA) may be helpful. If both of these methods result in negative findings but the patient has symptoms consistent with small bowel diarrhea/malabsorption, upper endoscopy with biopsies and duodenal aspirate can be considered.
Stool culture is not routinely used because of the difficulty of reproducibly isolating Giardia from patient fecal samples. However, stool cultures are beneficial in excluding other pathogens as the cause of a patient's symptoms.
Routine laboratory tests (eg, complete blood cell count, electrolyte levels) are often unremarkable. Eosinophilia is a rare feature of giardiasis.
Because immunoglobulin G (IgG) levels remain elevated for long periods, they are not beneficial in making the diagnosis of acute giardiasis. Serum anti-Giardia immunoglobulin M (IgM) can be beneficial in distinguishing between acute infections and past infections.
No imaging studies are required in the workup of giardiasis. Small-bowel plain films may show nonspecific thickening and distortion of the mucosal folds of the duodenum and jejunum, hypersecretion, and hypermotility. [13, 45] These changes are reversible with therapy. Barium studies should be avoided because barium can obscure identification of parasites for as long as 10 days.
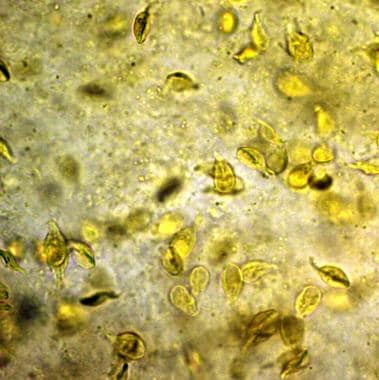
Stool Examination
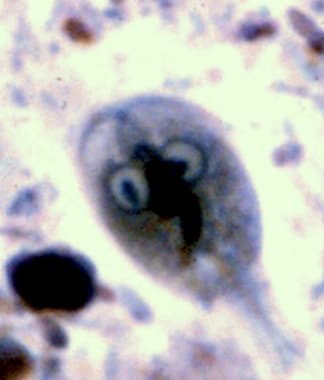
Stool examination (see the images below) for trophozoites or cysts is the traditional method for diagnosing giardiasis. At least three stools taken at 2-day intervals should be examined for ova and parasites. Trophozoites may be found in fresh, watery stools but disintegrate rapidly. If the stool is not fresh, or if it is semiformed—formed, trophozoites will not be found.
Cysts are passed in soft and formed stools. Fresh stool can be mixed with an iodine solution or methylene blue and examined for cysts on a wet mount. If not immediately examined, stool should be preserved in polyvinyl, alcohol, or 10% formalin, with subsequent trichrome or iron hematoxylin staining. Cyst passage is variable, not related to clinical symptoms, and may lag behind the onset of symptoms by a week or more.
Cysts are smooth walled and oval, measuring 8-12 μm long and 7-10 μm wide. Iodine stains the cysts brown and accentuates their intracystic structures, particularly their curved median bodies, axonemes, and nuclei. By focusing through the plane of the sample, four nuclei may be visualized, representing two daughter trophozoites.
Trophozoites are leaf-shaped, measuring 9-21 μm long and 5-15 μm wide. Stained organisms have a characteristic facelike image with two nuclei and four pairs of flagella. [31]
Because many antibiotics, enemas, laxatives, and barium studies mask or cause the disappearance of parasites from the stools, microscopic examination should be postponed for 5-10 days following these interventions.
Fecal leukocytes should not be visualized in stool samples of patients with giardiasis.
Stool Antigen Detection
Several tests to detect Giardia antigen in the stool are commercially available. [15, 45, 68] These utilize either an immunofluorescent antibody (IFA) assay or a capture enzyme-linked immunosorbent assay (ELISA) against cyst or trophozoite antigens. These tests have a sensitivity of 85-98% and a specificity of 90-100%.
Polymerase chain reaction (PCR) techniques may detect giardia in stool samples with parasites concentrations as low as 10 parasites/100 mcL. PCR may also be a valuable tool for screening of water supplies. [69] Real-time PCR has also the advantage of being able to detect both mild and asymptomatic infections. [70]
While more sensitive than stool examination, these examinations are limited to the detection of Giardia; isolated use might result in missing an alternative or concurrent parasitic infection.
A 2009 study evaluated a screening test for Giardia and Cryptosporidium on 136 fecal samples. The results showed the test to be 98.4% sensitive and 100% specific; the positive and negative predictive values were 98.7% and 99.3%, respectively. [71]
String Test
The string test (Entero-test) consists of a gelatin capsule containing a nylon string with a weight attached to it. The patient tapes one end of the string to his or her cheek and swallows the capsule. After the gelatin dissolves in the stomach, the weight carries the string into the duodenum.
The string is left in place for 4-6 hours or overnight while the patient is fasting. After removal, it is examined for bilious staining, which indicates successful passage into the duodenum. The mucus from the string is examined for trophozoites in an iodine or saline wet mount or after fixation and staining.
Other Tests
Fecal fat quantification or a qualitative fecal fat analysis with Sudan stain may confirm steatorrhea. Serum carotene, folate, and vitamin B-12 levels may be variably depressed as a result of malabsorption. The findings from D-xylose absorption tests may be abnormal.
Disaccharidase deficiency is common during and after treatment and can be diagnosed with the aid of a lactose tolerance breath test. [72]
Serum electrophoresis can help diagnose immunoglobulin A, immunoglobulin M, and, occasionally, immunoglobulin G deficiency states.
Serologic studies are being investigated.
Endoscopy and Biopsy
Esophagogastroduodenoscopy (EGD) may be employed in patients in whom the diagnosis is suspected but unproven after stool microscopy and ELISA. This also may be used for patients who continue to manifest symptoms of malabsorption after adequate therapy.
Endoscopy may be used to assess the small bowel architecture and obtain a duodenal aspirate or biopsy. While rarely necessary, duodenal biopsy may be the most sensitive test. This has several benefits over the string test. An aspirate can be cultured to assess for overgrowth of the small intestine. Other small bowel parasites, such as microsporidia and cryptosporidia, may be detected in biopsy samples. Spruelike lesions, which may occur with giardiasis, can be detected with this technique.
Biopsy can also be used to visualize changes in histologic features. Intestinal biopsy shows flattened, mild lymphocytic infiltration and trophozoites on the surface. [27, 34]
Biopsy specimens from duodenum are often teeming with sickle-shaped Giardia trophozoites, which are tightly bound by the concave attachment disc to the villus surface of the intestinal epithelial cells. In cases where trophozoites are difficult to recognize in biopsy samples, specific anti-Giardia immunoperoxidase stains aid in the detection of the organisms, although these stains are not readily available.
Many patients exhibit atrophy of the small intestinal villi with a mixed inflammatory infiltrate in the lamina propria. The brush borders of the surface absorptive epithelial cells are irregular, and virtual absence of villi may be noted, as in celiac disease.
Histologic Findings
No classic universal histologic abnormalities result from infection with G intestinalis. Patients with giardiasis who undergo endoscopy and small bowel biopsy are likely to have similar findings compared to controls.
Patients with immunoglobulin deficiency states and giardiasis may demonstrate various degrees of villous atrophy that bear a striking resemblance to celiac sprue. These conditions can be differentiated from sprue by the absence of plasma cells in the lamina propria.
-
Giardiasis. Giardia lamblia, cyst form.
-
Giardiasis. Giardia lamblia trophozoites in culture.
-
Giardiasis. A Giardia intestinalis cyst.
-
Giardiasis. Giardia intestinalis trophozoites on stool examination from a patient with diarrhea.
-
Giardiasis. Giardia trophozoite.
-
Giardiasis. Giardia cyst.